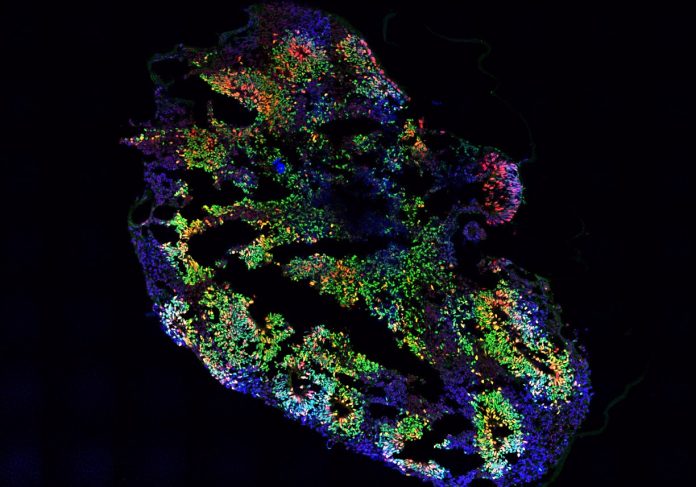
A slice of a brain organoid, PC: Pavithra L Chavali
We have all taken a pill when we fall sick, but have you wondered how medicines are developed? The research and development of each medicine can take almost 10 years, including the initial discovery of a candidate molecule in the lab using cell culture, followed by the testing of its safety and efficacy in different animal models. Three rounds of human clinical trials then ensue, where the medicines are tested in few hundreds to thousands of humans to test the efficacy and presence of any adverse effects in the human population.
While this has been the conventional method of drug development, 90% of clinical drug development fails, where only one of every 10 drugs that enter the clinical trials finally enters the market. One of the reasons for this high failure rate has been attributed to the inability of animal models to accurately capture and predict the human responses to pathogens and drugs.
A well-known example has been the animal studies on Amyotrophic Lateral Sclerosis (ALS), a fatal disease that leads to the loss of neurons that control our motor functions. This often leads to wasting of muscles, paralysis, and death. When this disease was studied using mice models, they also showed wasting of muscles; however, death in these mice was caused by a blockage in the gut. This indicated different mechanisms underlay how the disease manifested and acted in animals versus humans. Many studies like these show the need for developing model systems that are based on human cells and can better capture the complexities of human biology.
Recent scientific advancements have led to the creation of model systems, such as organoids and organs-on-chip. These are based on human stem cells and aim to mimic the physiology and functions of a single human organ or a network of organs at a smaller scale.
Organoids are three-dimensional miniature versions of human organs, built from stem cells, which can help scientists study human organs in a lab. When stem cells are cultured with certain growth factors, the process stimulates stem cell differentiation into various specialized organ cell types. A collection of such various cell types self-organizes in a spatial resolution that is very similar to what is observed in the human body. Due to their three-dimensional structure harboring diverse cell types, organoids have an edge over routine cell culture that is mostly monolayered and lacks representation. Scientists worldwide have developed various organoids, including liver, lungs, brain, and heart organoids.
Organs-on-chip, another type of human-biology-based model system, are microdevices consisting of a clear flexible rectangular polymer, the size of an AA battery. This polymer contains hollow channels that are lined with cells of human organs and blood vessels, thus presenting a cross-section of a living human tissue/organ. As we can mimic the blood flow and tissue-tissue interactions in organ-on-chip devices, you can imagine how powerful these could be to understand the nitty-gritty of diseases such as clogged arteries, and tuberculosis in the lung, and even side effects of drugs on the kidney!
These organoids and organ-on-chip systems aim to replicate the physiology of human systems at the micro-level, hence they are also called “microphysiological systems”. These systems are currently being used to study both the normal structure and function of human organs, as well as what happens when they’re diseased. One could also study the effect of toxic substances, pathogens, or candidate drugs on human organs using these systems.
While these systems may sound futuristic, they are already being used in the field of human disease research and drug development globally. For example, in one study organoids were created using cells from patients with pancreatic duct adenocarcinoma and various drug candidates were tested on these organoids. Patients who were treated with the candidate drugs shortlisted based on the response in organoids had a better survival rate. Similarly, infection from the Zika virus in pregnant women is characterized by microcephaly, a birth defect where a baby’s head is smaller than expected. One of the first pieces of evidence of the link between the Zika virus and microcephaly was found using brain organoids.
However, there remain challenges in developing these systems as exact replicas of human organs and systems. These are currently areas of intense investigation, such as the incorporation of the immune system, vasculature, and microbiota in these systems. Also, inside the human body, organs and tissues exist in an interconnected state, rather than isolated organs or tissues. Researchers are now trying to connect various individual organs on-chip. This integrated system is referred to as “human-on-a-chip”, and can provide immense insights into how an integrated network of organs respond to drugs or pathogens.
Nevertheless, the use and development of these systems are on an exponential rise in various research labs and biotech companies, globally as well as in India. The vast leaps in research and technology development in the last decade position these models as the next frontier of human-based biomedical research and drug discovery.