In order to find a potential cure or vaccine for COVID-19, it is necessary to grow the novel coronavirus in large quantities in safe and contained laboratory settings. In the last few months, institutes around the country, including CSIR-Centre for Cellular and Molecular Biology (CCMB), Hyderabad, and National Institute of Virology (NIV), Pune, have joined the effort to grow the virus. Somdatta Karak from CCMB provides us with a first-hand peek inside one such laboratory.
On a hot, sultry, and a rather quiet afternoon amidst the COVID-19 scare, I am on my way with Dhiviya Vedagiri to the Biosafety Level‑3 (BSL‑3) lab at CSIR-Centre for Cellular and Molecular Biology (CCMB) where she and others have been growing SARS-CoV‑2, the coronavirus responsible for the COVID-19 pandemic.
Dhiviya, a PhD student with Krishnan H Harshan, works on understanding the interplay between flaviviruses and host immune responses. However, that is now on a temporary halt in order to channelize all efforts into the fight against COVID-19. Growing the virus is the first step towards developing vaccines against the virus as well as testing potential drugs.
The BSL‑3 is almost a sacred place – dedicated to culturing disease-causing infectious microbes. While growing non-pathogenic E. coli bacterial strains is a fairly commonplace activity in many life science labs, infectious ones need a plethora of safety rituals to be followed.
The journey to a BSL‑3 lab begins with a series of change rooms. Across these, the air pressure keeps dropping, and the amount of Personal Protective Equipment (PPE) on the entrant keeps increasing. A consistently lower air pressure than the outside change rooms (by 30Pa – not something that you would generally feel) ensures the potentially contaminated air from inside does not go into the change rooms. But the seriousness of the situation dawns upon you with the PPE – foot covers, special shoes, shoe covers, a lab coat followed by a surgical gown, gloves, a pair of goggles, an N95 mask and a head cover – all to ensure that no body part is exposed to even this “clean” air. The focus is on making sure that the researcher neither carries in any contamination from outside nor brings out an infection from the BSL‑3 while leaving.
Entering the BSL‑3 finally, we are greeted by bright light and shiny clean stainless steel furniture housed in a temperature and humidity-controlled lab. We don another pair of gloves and move towards the incubator where the SARS-CoV‑2 virus particles are growing on their host cells in little wells in a plate placed in a temperature-controlled incubator. The viruses are kept cosy at 37ᵒC with controlled amounts of CO2, their host cells sustained by a few millilitres of a tomato red coloured nutrient solution, supplemented with proteins and finished off with a dash of antibiotics to keep bacteria at bay.
A virus is a quasi-alive particle carrying minimal content with itself. Its genetic material is encapsulated within lipid and protein layers. It does not grow in size or metabolize nutrients, but it multiplies in number within a host whose protein machinery it can hijack for its own use. SARS-CoV‑2 can infect cells that express a certain set of proteins called ACE‑2. Here in the BSL‑3, they are offered ACE‑2 expressing kidney epithelial cells from the Green African monkey (sold as Vero cells) to grow on.
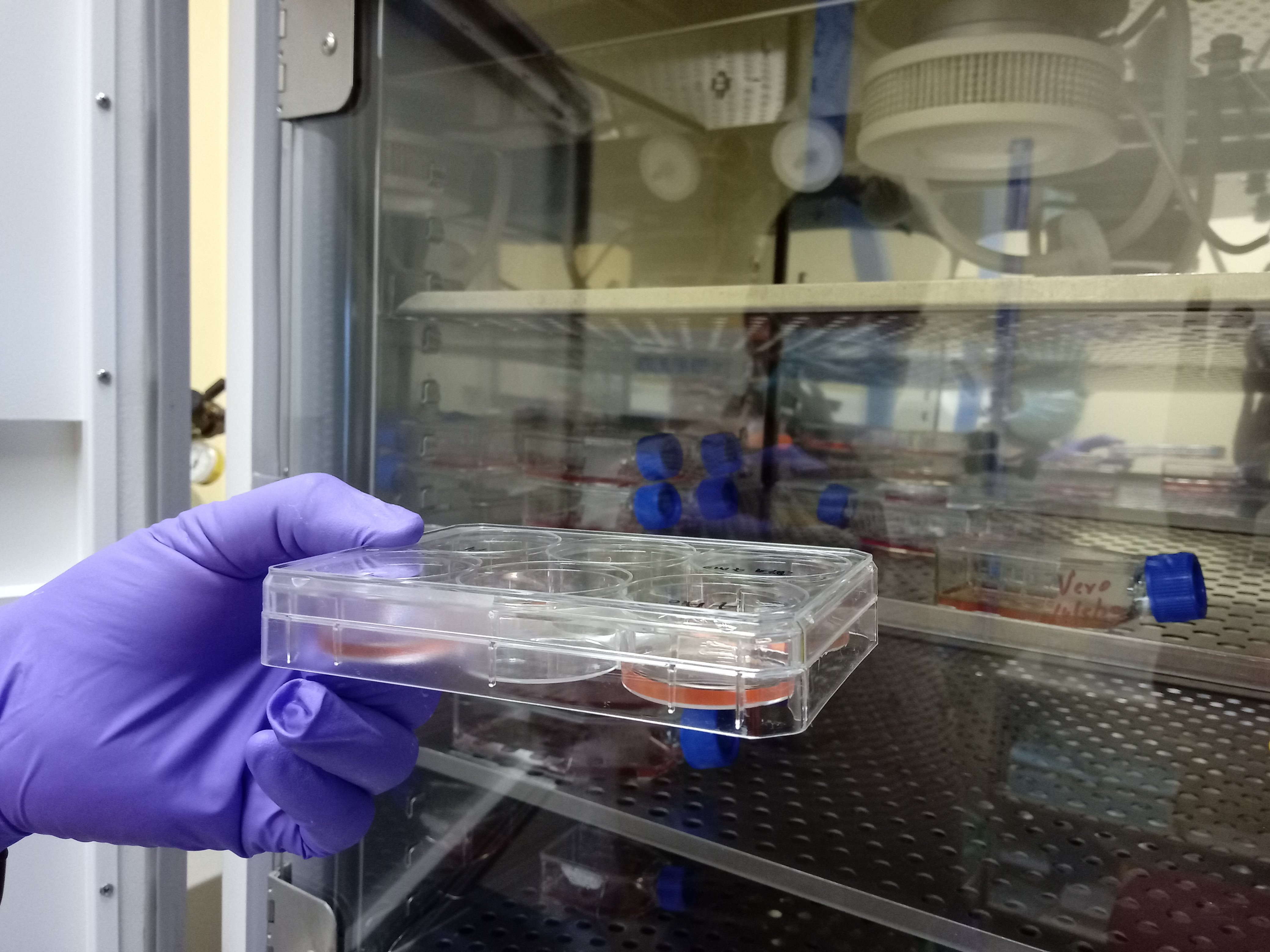
Dhiviya comes here every few days to see how the Vero cells infected with SARS-CoV‑2 are faring. A change in the colour of the nutrient solution indicates a change in the pH (acidity) of the solution. She would then need to monitor the CO2 settings in the incubator or add fresh medium. Today she takes out a 6‑well plate containing the Vero cells she had infected with a sample isolated from a COVID-19 patient a week back. The colour of the nutrient solution appearing fine, she places the plate under a microscope to check the health of the cells.
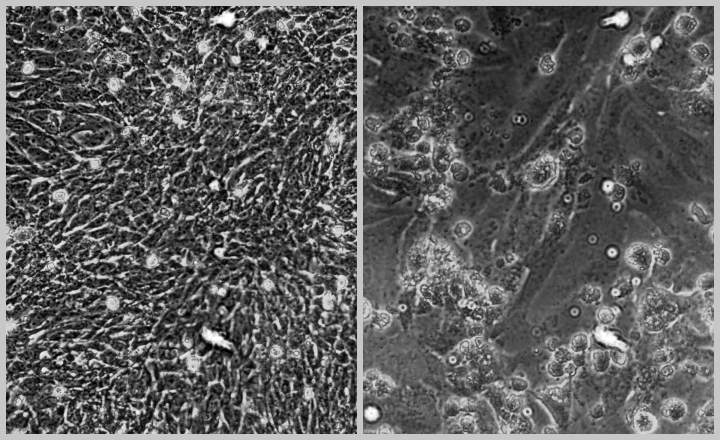
The Vero cells grow flat on the plate’s surface and appear irregular in shape. But most of the cells in the sample she is checking have lost contact with the surface and can be seen floating as globules. “These are dead cells,” she says. The viruses from the patient sample seem to have infected the Vero cells, killing them. It was now time to confirm it with RT-PCR.
RT-PCR allows researchers to check for the presence of the virus’ genetic material – its RNA — in a sample. RNA is made of four repeating subunits called nucleotides– adenine (A), uracil (U), cytosine ( C) and guanine (G). However, SARS-CoV‑2’s RNA sequences are far longer than most other RNA viruses with about 30,000 A, U, G and Cs. It is this sequence that is read by the host cell’s protein synthesis factories and used to make viral proteins. These new proteins then make many copies of the virus’s entire RNA to be packed inside lipid and protein membranes, which are released as new virus particles. The sequence of this RNA can mutate as the virus grows, and thus, alter its proteins – a part of its constant evolutionary arms race with its host. This change can sometimes alter the virus’s infectivity or the severity of disease symptoms it causes.
An effective vaccine against SARS-CoV‑2 would be one that targets most, if not all, COVID-19 causing strains. An effective drug testing platform would need as many of these strains to be grown and tested as possible. Both of these require millions of copies of the virus to be grown, collected from at least hundreds of patients to cover as many strain varieties as possible. It is an activity that is expected to take 2 – 3 months in the very least at CCMB to have a fair representation of the Indian coronavirus.
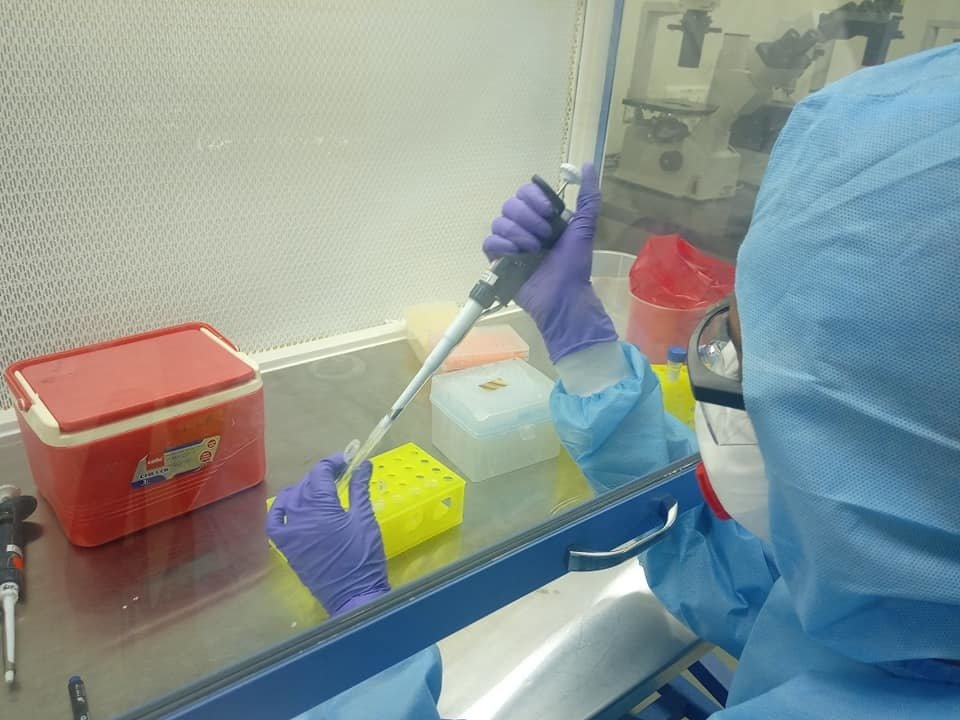
Dhiviya takes the 6 well-plate to a working hood which has a continuous exhaust with HEPA filters that trap the viruses before the air goes out. Times moves slowly here. Every step in the procedure begins with cleaning surfaces and equipment with bleach, alcohol, and UV radiation. A few hundreds of microlitres of the nutrient solution from the wells of infected and uninfected samples are collected into tubes. The virus has two protective layers – an outer lipid bilayer, and an inner protein capsid to which its RNA is bound. RT-PCR looks for this RNA. So, the protective layers have to be broken open.
Alcohol and detergents dissolve the lipid membrane and puncture the protein layers. Once the membranes are broken, the cell soup is gently transferred onto a bed that specifically binds the RNA. Dhiviya washes the bed to remove remnants of salt and alcohol as these might cause problems during RT-PCR. She then adds water to the bed to dissolve the RNA and collects it for running the RT-PCR reaction. The foremost concern here in what is otherwise a regular molecular biology lab practice is to avoid any risk of aerosol formation or spillage.
Now that the virus is broken down and hence inactive, the sample doesn’t need to remain under BSL‑3 conditions. Dhiviya puts the RNA sample dissolved in water in an enclosed chamber between BSL‑3 and the more relaxed BSL‑2 labs – called the “passbox”. Samples can be moved out of BSL‑3 only after they go through a final UV irradiation within the passbox itself. Then, with a final clean-up of her working surface and her equipment, complete with a dose of UV, Dhiviya and I finally move out of the BSL‑3.
Life without the PPE feels so much lighter and pleasant. The gowns, headcovers and goggles go for recycling — they would be treated with high temperature and pressure to kill any living organism on them (a process called ‘autoclaving’). The lab coats go for UV treatment, while the N95 masks, gloves, shoe and foot cover go into a discard bag. Any discard from the lab or the change area will be autoclaved before disposal.
I head for home, and Dhiviya catches some fresh air. Later in the evening, she runs the RT-PCR and checks if the samples show the same sequence of A, U, G and C that SARS-CoV‑2’s RNA contains. As I wrap up my dinner, Dhiviya’s message flashes on my phone – “The samples are positive.” One batch of the virus is now growing in the Vero cells, with many others in waiting to be eventually grown in quantities useful for vaccine development and drug testing.