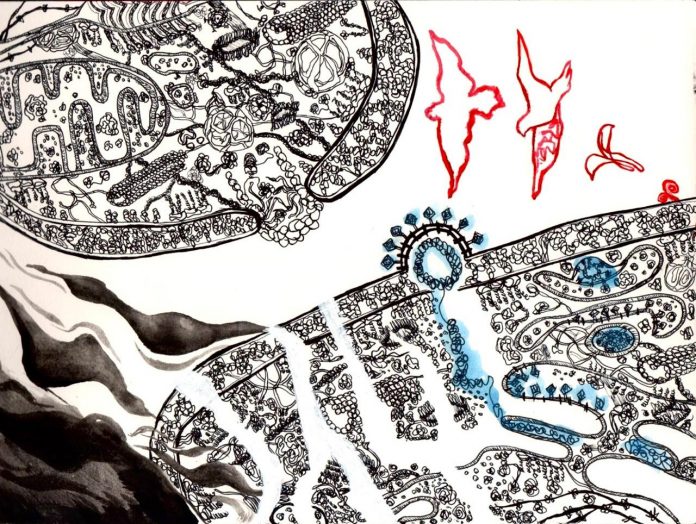
Messenger, by Greeshma Murthati
I am the first researcher in my family. I joined CCMB in August 2019 as a PhD student to study how we, humans, respond to viral infections. What started with the Japanese encephalitis virus and dengue virus moved to the COVID-19 causing coronavirus, SARS-CoV-2 within a year. When I called my parents to tell them that I will be working closely with the virus that was causing havoc all across the world, I couldn’t make them less worried. To be fair, they were right in their own standing. COVID-19 had imposed itself as one of the biggest threat to humankind in a while. Hundreds of thousands of people dying every day, with more people just desperately clinging to dear lives.
Amid all the confusion, I had soon become the unanimous leading authority for all COVID-19 related queries in my family. I started addressing people’s questions of many kinds. It ranged from knowing if the sound vibrations by chanting religious songs could kill the virus to if drinking alcohol would kill the virus to exercising and eating healthy to boost the immune system. Even specialised terms like interferon activity, cytokine storm, inflammation came into daily conversations of many people. Everyone wanted to know how to keep themselves safe from the virus.
But do we really know how the immune system protects out body against coronavirus, or any viral infections for that matter?
The body’s sentinel system
Our body is essentially a very complex composite made of layers of cells and tissues, which makes the organs. There are multiple physical and chemical barriers that prevent the entry of foreign pathogens into our bodies. Despite these barriers, microorganisms often invade our bodies. When they enter and thrive in our bodies, we become their hosts.
Most commonly, viruses enter host cells by hijacking the cell’s control on cargo trafficking in and out of the cell. Once they are in, they release their genomes into the cell, and make viral proteins from it. The viral proteins take over the host cell’s protein making machinery and promote its own growth.
Standing against the virus, is the host’s immune system. There are specialized immune cells such as neutrophils, dendritic cells, T-cells and B-cells that can identify foreign particles and mount a chemical reaction against them. These cells are designed to ingest foreign particles and degrade them. But in addition, we now realize other cells of our bodies have similar capacities.
The epithelial cells make the outermost layer of our body, and are the first in line to face any infection. If they are infected by a virus, they have ‘sensors’ that detect the viral genetic material. Many viruses’ genetic material differ from our cells’. The activated sensors send molecular signals to other compartments of the cell, and ultimately instruct the infected cell to produce and secrete interferons among other cytokine molecules. These warn the neighbouring uninfected cells of the viral infection. In anticipation, the nearby cells arm themselves with antiviral measures that ultimately helps them to keep a check on viral replication. These include having molecular scissors to cut the virus’ genetic material or stop it from functioning.
Given these many checkpoints, most of viruses have a tough time establishing infections in a healthy body.
However, SARS-CoV-2, as a virus with a short replicating time, could evolve at a pace that was impossible for human cells to keep up with. And, the virus evolved in a way that it delays or antagonizes the signaling process in the infected human cells. Human cells fail to produce interferons against the virus, giving it enough time to replicate rapidly. Many scientists like us are still trying to figure out how SARS-CoV-2 does that.
At the same time, an overdose of interferons has been detrimental and even fatal for many COVID-19 patients. Interferons not only act as a messenger about the danger of pathogen invasion, but it also can rewire the physiology of the cells. This includes changes in cellular metabolism, cell division and even cellular death. Because of these complications, it is of utmost importance that the process of interferon production is very tightly regulated. Otherwise it can do more harm than good. How SARS-CoV-2 manages to induce a cytokine storm in some cases and completely block interferon production in some cases is another mystery which scientists are still trying to figure out.
Immunity is not simply about attacking a foreign particle in the body. It is also about knowing when and how to stop that attack. It is also about ensuring least damage to our own self. These are areas of active and rigorous research, and I realize these are the questions that interest researchers and me. I hope when my family wants to know more about immunity now, they start asking these questions too.