The voyage of Aedes aegypti, by Greeshma Murthati
Come monsoons, and dengue takes the centre stage of infectious diseases in India. There were 2 lakh reported cases in India in 2022; five times higher than in 2020. Despite this surge, especially in urban and semi-urban areas, our understanding on dengue remains rather limited.
Dengue is a vector-borne viral disease that is caused by dengue virus (DENV). In mild cases, dengue is difficult to diagnose due to the absence of specific symptoms. But in some cases, it starts presenting symptoms like high fever, nausea, rash, muscle and joint pains. If not taken care of properly, dengue patients can show severe symptoms such as bleeding of gums, weakness, persistent vomiting. Left unchecked, the progression of the virus can be fatal too.
There are four different serologically distinct strains of dengue virus – DENV1, DENV 2, DENV3 AND DENV4. The term serologically distinct means that each strain would generate a different immune response than the other. Thus, the antibody that our body produces from getting infected with one strain of DENV might not protect us against another strain. This is what makes dengue more interesting and dangerous. This would mean that a person can have multiple dengue infections in their lifetime.
Dengue virus transmits to humans through the bites of female Aedes mosquito, preferably the Aedes aegypti mosquito. But why does dengue only transmit via Aedes mosquito even though there are more than 3500 species of mosquitoes present around the world? A part of the answer lies in evolution!

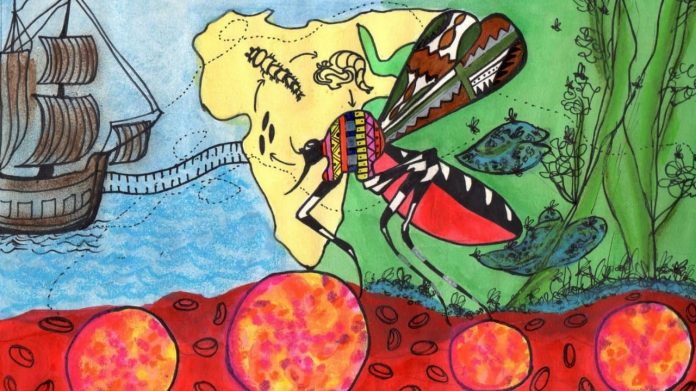
Aedes aegypti is native to African forests. Long back, humans started living in the forests and started to store water year around which makes perfect breeding grounds for Aedes aegypti as it grows in stagnant water bodies. During the sixteenth century, European ships stopped in Africa for slave trades, and very likely also picked up Aedes and dengue virus from there.
Chasing the origin of viruses is not very easy, especially DENV, given that dengue symptoms were difficult to unambiguously diagnose before modern medicine came into picture. The first case of dengue was recorded in early 1600s in the Caribbean and Panama, and interestingly, it was the same time when Yellow Fever and Aedes aegypti were introduced. Clear, unambiguous dengue cases with the symptoms that we know of now, were reported the first time almost simultaneously in Africa, Asia and Americas in 1779-1788.
As humans started migrating from African continent, they also carried the virus to different parts of the world with them. Probably due to the adaptation of Aedes aegypti to grow in stagnant water bodies and its capacity to lay eggs in difficult to reach areas in urban settings, it is one of the most prominently found mosquito species in the surroundings with human activities. .
There are some conditions that makes Aedes aegypti an efficient vector for DENV. It uses humans exclusively as a source of blood meals. It lives in high densities in close associations with humans over a wide range of geographical areas. And, it allows many human pathogens to grow in its saliva. All these allow these mosquitoes to easily infect humans with DENV. Not only that, Aedes aegypti is also the primary vector for other major viruses such as Yellow Fever Virus, Zika virus and Chikungunya virus.
What makes it possible for Aedes aegypti to harbour so many viruses, which also happen to be dangerous for humans? Scientists study both the mosquitoes and the viruses to find answers to it.
They have found that the Aedes aegypti’s immune system works in ingenious ways to avoid the mosquitoes getting sick when they are infected with the dengue virus while still allowing the virus to grow, and transmit to humans.
Small interfering RNA (siRNA)-mediated antiviral pathway is one of the most important and effective arsenals of insects against viral infections, especially the viruses with RNA as their genetic material. DENV, grows in the midgut of mosquitoes and replicates in heavy numbers there. Mosquitoes produce siRNA in their midgut as a response to DENV replication, and restricts the viral replication. In 2018, a group of scientists published a study where they showed that production of a protein called loqs2 in midgut is absolutely important for this siRNA mediated antiviral response against DENV. But Aedes aegypti does not produce this protein in midgut, and thus, allowing the virus to grow in the mosquitoes!
A study in 2022 showed that humans infected with dengue virus smelled more attractive to mosquitoes, thus, fostering the virus’ further spread. Another very recent study in 2023 also showed that mosquito saliva contains proteins that ease the dengue viruses infecting humans.
In addition to the evolutionary advantages that support the co-existence of dengue viruses and Aedes aegypti, these mosquitoes can also lay eggs that are resistant to drought conditions. This makes their spread even more effective geographically. It also has a tendency of feeding multiple times during one egg laying cycle, thus increasing the risk of infection to multiple people. Having said that, there are also limitations for Aedes aegypti; it cannot undergo winter diapause (a process similar to hibernation), which limits its spread to the more temperate regions. Its dispersal capacity is also limited in its adult form, with an estimated flight range of 200 meters. Can we use all of this to prevent the spread of dengue?
With so much urbanization and the mosquitoes’ adaptability to it, it is relatively difficult to isolate Aedes aegypti and dengue from human civilization. However, the governments worldwide are trying its level best to monitor, control and eradicate dengue through its programs, we also have to do our bit in order to contribute to it. Keeping the surroundings clean, avoiding storage of water in open containers, and maintaining proper routines of insecticide sprayings could limit its spread to a major extent. And, as our understanding grows on the behaviour and physiology of the mosquitoes and the viruses, novel strategies of treatment and control will come by too.