Cancer is the second leading cause of death worldwide. According to global cancer statistics 2022, nearly 20 million new cases were reported with the disease and almost 10 million lost their lives to it. These numbers are predicted to rise to 35 million by 2050. But why is cancer so fatal? The answer lies within the tiniest functional members of our body: cells.
From a healthy cell to a cancer cell
Every cell holds an instruction manual in the form of DNA — a blueprint that guides it to function, grow, and divide in an orderly fashion by producing the right proteins. However, the very ability of cells to grow and replicate comes with a cost. DNA, though resilient to changes, can sometimes be altered. These changes, or mutations, may result in faulty proteins that disrupt normal cell function.
The odds of a DNA sequence getting mutated are about 1 in 100,000. Fortunately, our cells are equipped with highly efficient DNA repair systems that quickly fix most errors. Damaged cells are often destroyed by the body’s own defense mechanisms. But on rare occasions, defective cells escape detection, multiply, and form an abnormal mass — a tumor.
A tumor becomes dangerous when it grows large enough to press on vital organs. If it invades nearby tissues, taking up space and consuming nutrients, and spreads to other parts of the body, it is classified as cancer.
The primary triggers for changes in the DNA and thus cancer can be environmental, biological, or lifestyle-related. Prolonged exposure to tobacco smoke, harmful radiation, or toxic chemicals can damage the DNA. Certain viral infections can also introduce mutations. An unhealthy lifestyle and chronic stress further strain the body, making DNA more vulnerable. Often, it’s a combination of these factors that sets cancer in motion.
Immunity against cancer
Our body is naturally equipped to defend against invading pathogens and other harmful agents, an ability known as immunity. This defense system is a highly coordinated, complex network of cells and molecules that detect and eliminate threats, keeping us healthy. It constantly performs surveillance, scanning for anything unusual. This same immune system is capable of detecting cancer cells. Those with weak immune systems have a higher risk of developing cancers.
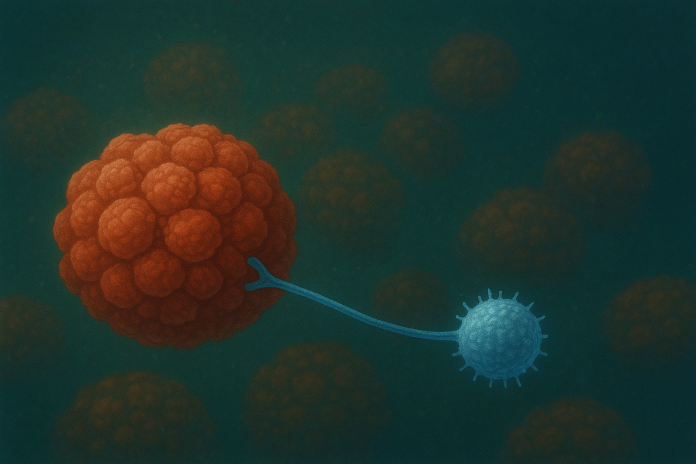
When a healthy cell turns cancerous, it displays special signals called tumor-associated antigens like ID tags, that warn and activate immune cells. For example, specialized fighter cells such as Natural Killer cells and T cells can recognize and destroy these tagged cells.
But cancer is a master of trickery. Over time, these sneaky cells evolve and learn multiple tactics to evade detection, hiding from the immune system for years before they resurface. This ability to adapt and survive is a trait rooted in evolution itself, that explains why cancer can recur even after treatments.
How do cancer cells evade the immune response?
One way cancer cells disguise themselves as normal cells, is by producing protein markers of normal cells in abundance. These false cues can confuse immune cells, exhaust them, creating physical barriers that prevent an effective attack.
Another strategy is the formation of a protective shield known as the tumor micro-environment. This specialized environment shelters cancer cells and blocks immune cells from infiltrating or recognizing them. As a consequence, immune surveillance is weakened, and tumor cells can thrive unchecked.
Adding to their defense, research shows that some cancer cells can steal mitochondria—the energy-producing powerhouses of cells, from T cells. This deprives the T cells of the energy they need, rendering them ineffective and reducing the body’s anti-tumor immunity.
Such advanced escape mechanisms employed by cancer cells have pushed scientists to develop newer treatment strategies. While traditional approaches such as surgery, radiation, and chemotherapy aim to directly remove or destroy cancer cells, modern immunotherapies are designed to reawaken and empower the immune system, enabling it to combat a wide range of cancers more effectively.
Choices of Immunotherapies
Immunotherapy includes a range of strategies to harness the body’s own defenses against cancer.
One approach is to keep immune cells active for longer by blocking the checkpoints that normally dampen their activity. This frees them to attack cancer cells more aggressively. Another involves administering highly specific antibodies that act like guided missiles, homing in on cancer cells. In some cases, viruses are genetically modified to infiltrate and destroy cancer cells from within—a method known as oncolytic virus therapy.
Despite their promise, immunotherapies also have some caveats. An overstimulated immune system can trigger excessive inflammation, damaging healthy tissues.
A more advanced option that can circumvent these challenges, effective even when other immunotherapies fail, is CAR T-cell therapy—short for Chimeric Antigen Receptor T-cell Therapy. In this treatment, a patient’s own T cells are collected and genetically engineered to produce a special chimeric receptor: part of it comes from antibodies that recognize cancer cells, and part from T-cell proteins. This receptor works like a GPS, locking onto tumor-specific antigens and enabling T cells to bind to and destroy only cancer cells. Once modified and tested for efficacy against the patient’s cancer cells, these cells are multiplied in the lab, and infused back into the patient. Inside the body, they continue to replicate, patrol, and eliminate cancer cells. These CAR T-cells can remain active in the body, sometimes, for years.
CAR technology is not limited to T cells; other immune cells such as dendritic cells and natural killer (NK) cells can also be adapted, leading to CAR-NK therapies. Overall, CAR technology paves a way to highly personalized treatments tailored to individual patients, a hallmark of precision medicine.
However, CAR-based therapies also come with a few challenges. Unlike many treatments, CAR T-cell therapy cannot be tested in animal models before human use. It is expensive—often costing up to 10 times more than conventional cancer treatments available today. They may still cause severe immune-related side effects in some patients. And, so far, they have no success against solid tumors. Currently, they are approved mainly for certain blood cancers, which are easier for immune cells to access because they circulate throughout the body.
Nevertheless, CAR T-cell therapy remains a powerful form of immunotherapy. Custom-designed for each patient, it mounts a stronger and more targeted attack against cancer. It typically requires only a single infusion and can offer long-term protection. With ongoing research and advancements, CAR-cell therapy holds great promise and may one day replace conventional chemotherapy as a front line cancer treatment.